The Eukaryotic Cell Cycle⁚ A Foundation
The eukaryotic cell cycle‚ a fundamental process in all eukaryotic organisms‚ governs cell growth‚ replication‚ and division. This intricate cycle comprises distinct phases⁚ G1‚ S‚ G2‚ and M‚ each meticulously regulated to ensure accurate DNA duplication and chromosome segregation. Disruptions in this tightly controlled process can lead to uncontrolled cell proliferation‚ a hallmark of cancer development. Understanding the cell cycle is crucial for comprehending the mechanisms underlying cancer initiation and progression.
Phases of the Eukaryotic Cell Cycle
The eukaryotic cell cycle is a complex‚ multi-stage process that ensures accurate duplication and distribution of genetic material. It is broadly divided into two major phases⁚ interphase and the mitotic (M) phase. Interphase‚ the longest phase‚ consists of three sub-phases⁚ G1 (Gap 1)‚ S (Synthesis)‚ and G2 (Gap 2). During G1‚ the cell grows and carries out normal metabolic functions‚ preparing for DNA replication. The S phase marks the crucial period of DNA replication‚ where each chromosome is duplicated to form two sister chromatids. G2 allows the cell to further grow and synthesize proteins necessary for mitosis. The M phase encompasses mitosis‚ the process of nuclear division‚ where duplicated chromosomes are separated and distributed into two daughter nuclei‚ followed by cytokinesis‚ the division of the cytoplasm‚ resulting in two genetically identical daughter cells. Precise regulation at each stage is essential; errors can lead to genomic instability and potentially cancer.
Regulation of the Cell Cycle
The intricate choreography of the eukaryotic cell cycle is governed by a complex network of regulatory proteins‚ primarily cyclin-dependent kinases (CDKs) and cyclins. CDKs are enzymes that phosphorylate target proteins‚ driving the cell cycle forward. Their activity is tightly controlled by cyclins‚ proteins whose levels fluctuate throughout the cycle. Different cyclin-CDK complexes govern transitions between specific phases. For instance‚ cyclin D-CDK4/6 complexes are crucial for progression through the G1 phase‚ while cyclin E-CDK2 initiates DNA replication in the S phase. Cyclin A-CDK2 and cyclin B-CDK1 regulate the G2/M transition and mitosis‚ respectively. This intricate system ensures that each phase is completed accurately before the next begins. Furthermore‚ checkpoints monitor DNA integrity and ensure proper chromosome alignment‚ preventing errors that could lead to genomic instability and potentially cancer. These regulatory mechanisms are essential for maintaining genomic stability and preventing uncontrolled cell growth.
Cell Cycle Checkpoints and Their Significance
The eukaryotic cell cycle incorporates several critical checkpoints acting as surveillance mechanisms to ensure accurate and error-free progression. These checkpoints‚ strategically positioned at the G1‚ G2‚ and M phases‚ meticulously assess the cell’s readiness to advance to the next stage. The G1 checkpoint‚ also known as the restriction point‚ evaluates cell size‚ nutrient availability‚ and DNA integrity before committing to DNA replication. The G2 checkpoint verifies the successful completion of DNA replication and the absence of significant DNA damage before initiating mitosis. Finally‚ the M checkpoint‚ or spindle checkpoint‚ ensures proper chromosome alignment on the metaphase plate prior to anaphase‚ guaranteeing accurate chromosome segregation into daughter cells. Dysfunction in these checkpoints compromises the cell cycle’s integrity‚ allowing cells with damaged DNA or improperly segregated chromosomes to proceed‚ increasing the risk of genomic instability and ultimately contributing to cancer development. Their significance lies in their role as gatekeepers‚ preventing the propagation of genetic errors and maintaining cellular homeostasis.
Cancer⁚ Uncontrolled Cell Growth
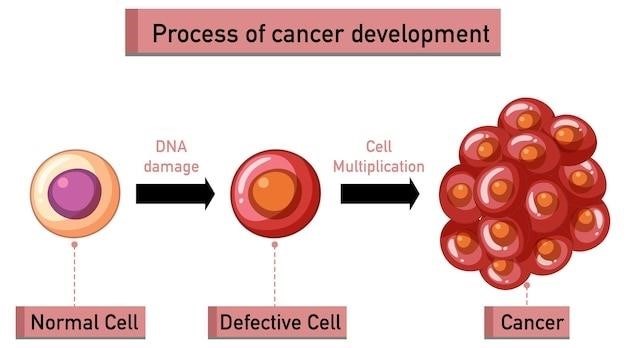
Cancer arises from uncontrolled cell proliferation‚ a consequence of dysregulated cell cycle control. This aberrant growth leads to the formation of tumors‚ masses of abnormal cells that can invade surrounding tissues and metastasize to distant sites. Genetic mutations play a central role in disrupting the normal cell cycle regulation‚ leading to cancerous transformation.
The Role of Cell Cycle Dysregulation in Cancer
The eukaryotic cell cycle‚ a tightly regulated series of events leading to cell division‚ is fundamentally disrupted in cancer. Normal cells possess intricate checkpoints that monitor DNA integrity and ensure accurate chromosome segregation. However‚ in cancer cells‚ these checkpoints often malfunction‚ allowing cells with damaged DNA to proceed through the cell cycle unchecked. This leads to the accumulation of genetic errors‚ further fueling uncontrolled proliferation. Mutations in genes encoding key cell cycle regulators‚ such as cyclins and cyclin-dependent kinases (CDKs)‚ contribute significantly to this dysregulation. Oncogenes‚ mutated versions of genes that normally promote cell growth‚ can become persistently activated‚ driving excessive cell division. Conversely‚ tumor suppressor genes‚ which normally inhibit cell cycle progression or promote apoptosis (programmed cell death)‚ may be inactivated‚ removing brakes on uncontrolled growth. The interplay between these oncogenes and tumor suppressor genes creates a perfect storm for uncontrolled cell division‚ a defining characteristic of cancer.
Oncogenes and Tumor Suppressor Genes
The delicate balance between cell growth and inhibition is maintained by a complex interplay of oncogenes and tumor suppressor genes. Proto-oncogenes‚ normal genes involved in regulating cell growth and division‚ can mutate into oncogenes‚ effectively becoming “accelerators” of the cell cycle. These oncogenes can lead to excessive cell proliferation by producing excessive amounts of growth-promoting proteins or by creating proteins with enhanced activity. Conversely‚ tumor suppressor genes act as “brakes‚” restricting cell growth and promoting apoptosis (programmed cell death) when necessary. Mutations in these genes‚ often caused by deletions or insertions‚ can disable their function. This loss of control allows damaged cells to survive and multiply‚ contributing significantly to cancer development. The combined effect of activated oncogenes and inactivated tumor suppressor genes creates a cellular environment conducive to unrestrained growth and the formation of cancerous tumors. Understanding the roles of these genes is critical in developing targeted cancer therapies.
Types of Cancer and Their Cellular Origins
Cancer is not a single disease but a collection of diverse diseases‚ each originating from different cell types within the body. Carcinomas arise from epithelial cells‚ lining organs and cavities‚ and represent the most prevalent type of cancer. Sarcomas develop from connective tissues such as bone‚ muscle‚ and cartilage. Leukemias are cancers of the blood-forming tissues‚ affecting white blood cells‚ red blood cells‚ and platelets. Lymphomas originate in the lymphatic system‚ part of the body’s immune defense. Myelomas specifically involve plasma cells in the bone marrow. The cellular origin profoundly influences the cancer’s behavior‚ response to treatment‚ and prognosis. For instance‚ the rapid proliferation of leukemia cells contrasts sharply with the slower growth of some solid tumors. Understanding the cell of origin is crucial for accurate diagnosis‚ effective treatment strategies‚ and predicting the clinical course of the disease. This cellular diversity underscores the complexity of cancer research and necessitates tailored approaches to treatment and prevention.
Investigating the Link Between Cell Cycle and Cancer
Research into the cell cycle’s role in cancer employs various techniques‚ including molecular biology‚ genetic analyses‚ and advanced imaging. These methods help pinpoint specific genes and proteins involved in cell cycle regulation and their dysregulation in cancer. Understanding these mechanisms is pivotal for developing targeted therapies.
Methods for Studying Cell Cycle Progression
Investigating the intricacies of the cell cycle and its deregulation in cancer necessitates a multifaceted approach. Flow cytometry‚ a powerful technique‚ allows researchers to analyze the DNA content of a large population of cells simultaneously. This enables precise quantification of cells in different phases of the cycle‚ revealing potential disruptions in progression. Immunofluorescence microscopy offers a complementary method‚ utilizing specific antibodies to visualize key cell cycle proteins within individual cells. This approach provides valuable insights into the localization and expression levels of proteins driving cell cycle progression. Furthermore‚ advanced imaging techniques‚ such as time-lapse microscopy‚ allow real-time observation of cell cycle events‚ providing dynamic insights into the temporal regulation of this intricate process. These diverse methodologies‚ often employed in concert‚ are crucial for unraveling the complexities of cell cycle regulation and its dysregulation in cancer development and progression.
Markers of Cell Proliferation and Cancer
Identifying reliable markers of cell proliferation is crucial for both understanding normal cell cycle dynamics and detecting cancerous transformations. Ki-67‚ a nuclear protein expressed exclusively in proliferating cells‚ serves as a robust marker of cell division and is widely used in cancer diagnosis and prognosis. Its presence indicates active cell cycle progression‚ while its absence suggests quiescence or cell cycle arrest. Another valuable marker is proliferating cell nuclear antigen (PCNA)‚ a protein involved in DNA replication. Elevated PCNA levels signify increased DNA synthesis‚ a hallmark of rapid cell growth often associated with cancer. Bromodeoxyuridine (BrdU)‚ a thymidine analog incorporated into newly synthesized DNA‚ provides a direct measure of DNA replication rates. By incorporating BrdU into cells and detecting its presence‚ researchers can quantify the proportion of cells actively replicating their DNA. These markers‚ individually or in combination‚ offer valuable insights into the proliferative state of cells‚ providing critical information for cancer detection‚ monitoring treatment responses‚ and predicting patient outcomes. The precise selection of markers depends on the specific research question and the type of cancer under investigation.
Therapeutic Targets Based on Cell Cycle Understanding
A deep understanding of the eukaryotic cell cycle has yielded several promising therapeutic targets for cancer treatment. The cell cycle’s intricate regulatory mechanisms‚ involving cyclin-dependent kinases (CDKs) and their associated cyclins‚ present attractive avenues for intervention. CDKs drive cell cycle progression‚ and their dysregulation in cancer makes them prime targets for therapeutic agents. CDK inhibitors‚ designed to block CDK activity‚ can halt uncontrolled cell proliferation. Furthermore‚ checkpoints within the cell cycle‚ responsible for monitoring DNA integrity and ensuring accurate chromosome segregation‚ are also potential therapeutic targets. Disrupting these checkpoints can sensitize cancer cells to chemotherapy or radiation‚ enhancing treatment efficacy. Another approach involves targeting specific proteins involved in DNA replication or repair‚ thereby hindering cancer cell growth and survival. Moreover‚ understanding the molecular pathways that regulate apoptosis (programmed cell death) enables the development of therapies that either stimulate apoptosis in cancer cells or prevent cancer cells from evading apoptosis. The continued exploration of cell cycle mechanisms will undoubtedly uncover further therapeutic targets‚ leading to the development of more effective and targeted cancer treatments.

Further Research and Clinical Implications
Further research into the intricacies of the eukaryotic cell cycle promises significant advancements in cancer diagnosis‚ prognosis‚ and treatment. A deeper understanding of cell cycle regulation‚ particularly the roles of various proteins and signaling pathways‚ is crucial. This includes investigating the complex interplay between genetic mutations‚ epigenetic modifications‚ and environmental factors in influencing cell cycle control. Advanced imaging techniques and high-throughput screening methods are essential for identifying novel therapeutic targets and biomarkers for early cancer detection. The development of personalized medicine approaches‚ tailoring treatments to individual patients based on their specific tumor’s cell cycle characteristics‚ holds immense potential. Furthermore‚ exploring the efficacy of combination therapies‚ integrating cell cycle-targeted drugs with other cancer treatments‚ needs further investigation. Clinical trials evaluating novel cell cycle-modulating agents are essential for translating research findings into improved patient outcomes. The ongoing pursuit of knowledge in this area will undoubtedly lead to more effective and less toxic cancer therapies‚ improving the lives of countless individuals affected by this devastating disease.